As part of a study involving 206 monozygotic and dizygotic twin pairs, researchers conducted a series of clinical and neuropsychological tests, showing how amyloid pathology is the subject of moderate genetic influence, indicating a major environmental contribution amenable to treatment.
The study appeared in the Journal of Neurology, Neurosurgery & Psychiatry.
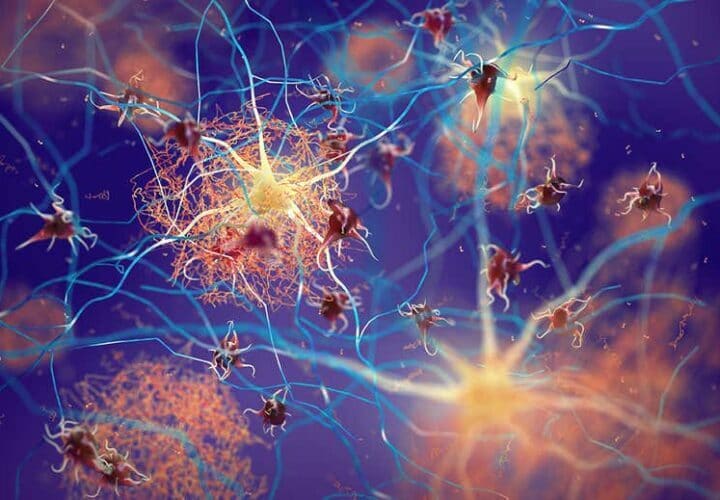
According to researchers at UNSW Sydney’s Centre for Healthy Brain Aging (CHeBA), the protein amyloid is involved in the early development of Alzheimer’s disease through its accumulation in the brain. Since the heritability of amyloid is moderate, genes only play a moderate role in establishing the variation in amyloid build-up within the brain.
One co-author of the study commented the following on the findings, “This is significant, because it tells us that whilst genes are important, there is actually a major environmental contribution that may respond well to intervention.”
“With respect to modifiable risk factors, we examined whether vascular risk factors such as hypertension, diabetes, high cholesterol, or a history of heart disease were significantly associated with amyloid burden or had any shared genetic basis.”
Researchers believe further research that helps to identify modifiable risk factors able to result in effective interventions for reducing amyloid build-up is warranted.
“Identifying modifiable risk factors will lead us to interventions that reduce the risk of amyloid accumulation—and ultimately risk reduction of developing Alzheimer’s disease,” researchers suggested.