What are beta-amyloids and what effect do they have on the brain? For this article, let’s take a comprehensive look at a phenomenon purportedly linked to cognitive disorders.
What Are Amyloids?
Simply put, amyloids are aggregates of proteins that have a fibrillar morphology and typically measure anywhere between 7 and 13 nanometers in diameter.
Based on a wealth of studies conducted over many years, amyloids are thought to contribute in some way to the onset of diseases, mostly affecting the brain. Some researchers feel that amyloids may be linked to amyloidosis and certain neurodegenerative diseases that are said to cause cognitive decline. Although time and time again, studies imply that amyloid pathologies may contribute to the development of cognitive disorders, there is no solid evidence to support this claim. It is currently the subject of intense research.
At the time of this article’s publication, more than three dozen proteins are thought to form amyloid in pathology. They are all related, to some degree, to a number of diseases. Such proteins include the following:
- ABri peptide
- ADan peptide
- Apolipoprotein C-II
- Apolipoprotein C-III
- Atrial natriuretic factor
- Beta-2 microglobulin
- C-terminal fragments of TGFBI/Keratoepithelin
- C-terminally extended Apolipoprotein AII
- Calcitonin
- Corneodesmosin
- Enfuvirtide
- Fibrinogen alpha chain
- Galectin-7
- Gelsolin
- Huntingtin exon 1
- IAPP (Amylin)
- Immunoglobulin heavy chains
- Immunoglobulin light chains
- Insulin
- Lactadherin / Medin
- Lactotransferrin / Lactoferrin
- Leukocyte cell-derived chemotaxin-2 (LECT-2)
- Lysozyme
- Microtubule-associated protein tau
- N-terminal fragments of Apolipoprotein AI
- N-terminal fragments of Apolipoprotein AIV
- N-terminally truncated Cystatin C
- Odontogenic ameloblast-associated protein
- Prolactin
- Proteins S100A8/A9
- PrP
- Pulmonary surfactant-associated protein C (SP-C)
- Semenogelin-1 (SGI)
- Serum amyloid A protein
- Transthyretin
- β amyloid peptide (Aβ) via Amyloid precursor protein
- α-synuclein
What Are Beta-Amyloids?
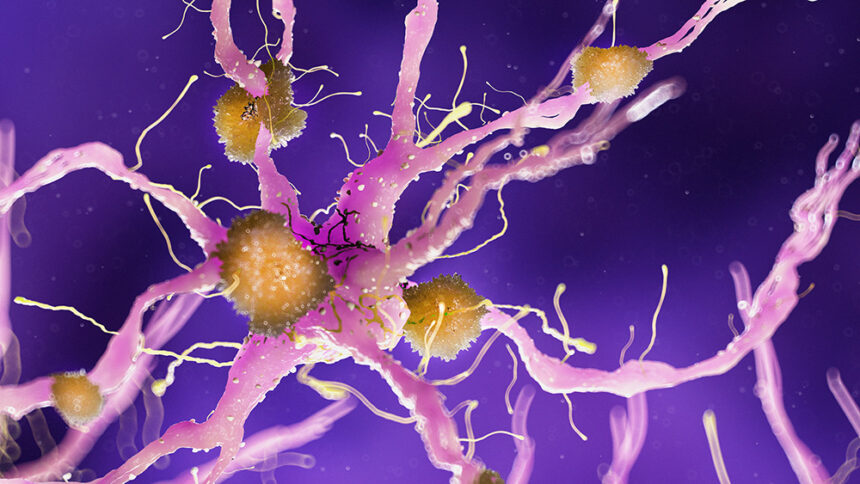
Beta-amyloids are a metabolic waste product that can accumulate in the intercellular fluid of the brain. Some experts assume that an accumulation of beta amyloid is related to a decline in brain function and the development of Alzheimer’s disease (AD). In patients with Alzheimer’s, beta-amyloid aggregates to form amyloid plaques, which interfere with the communication between neurons or brain cells.
When beta-amyloid protein fragments accumulate, amyloid plaques are produced. When the amyloid precursor protein (APP) is degraded, beta-amyloid is formed. APP has 771 amino acids and is broken down by two enzymes to generate beta-amyloid.
Amyloid Pathology
Amyloid pathology generally involves the 36–43 amino acid peptides that make up the majority of the amyloid plaques observed in the brains of patients with cognitive disorders, such as Alzheimer’s. The peptides are produced from the amyloid precursor protein, which is broken down by beta and gamma secretases to form Aβ in a cholesterol-dependent process and substrate presentation.
Aβ molecules may assemble into flexible, soluble oligomers that can exist in a variety of forms. It is currently suspected that some misfolded oligomers might drive other Aβ molecules to adopt the same misfolded oligomeric state, resulting in a chain reaction resembling a prion infection. Nerve cells are toxic to oligomers. Tau protein, the other protein theoretically involved in AD, also produces misfolded oligomers like prions, and there is some evidence that misfolded Aβ can stimulate tau to misfold.
The Theory of Amyloids
According to some researchers, soluble oligomeric forms of the peptide may have a role in the onset of Alzheimer’s. As per common belief, Aβ oligomers are the most toxic. Many genetic, cell biology, biochemical, and animal studies agree with the idea that Aβ plays a significant part in the pathogenesis of neurogenerative disorders such as Alzheimer’s.
The majority of researchers agree with the “amyloid hypothesis” that plaques are responsible for the pathophysiology of Alzheimer’s, although it has not been completely proven. An alternate theory holds that amyloid oligomers, not plaques, are the cause of the illness.
The amyloid hypothesis is seemingly intriguing because the gene for the amyloid beta precursor APP is situated on chromosome 21, and by age 40, individuals with trisomy 21, often known as Down syndrome, who have an extra gene copy display Alzheimer’s problems.
The hypothesis alludes to the cytotoxicity of mature aggregated amyloid fibrils, which are thought to be the toxic form of the protein responsible for altering the calcium ion homeostasis of the cell and initiating mortality. This notion is reinforced by the finding that higher levels of a type of beta amyloid protein known to form fibrils quicker in vitro correlate with earlier onset and more severe cognitive impairment in animal models and with the diagnosis of AD in people. However, mechanisms for the induced calcium influx or alternate cytotoxic processes proposed by mature fibrils are not immediately evident.
Amyloids and Alzheimer’s Disease
As emphasized throughout this article, amyloid pathology is hypothesized by some experts to be associated with Alzheimer’s disease. Some researchers believe tau protein, and not amyloid beta, may be the cause of Alzheimer’s symptoms.
The brain is widely believed to shrink to a certain extent as part of the healthy aging process. However, neurons are not damaged in enormous numbers. When a patient suffers from Alzheimer’s disease, however, enormous neuronal malfunction and widespread neuronal damage ensue. Thus, the loss of neuronal connections in the brain has an effect on memory and other cognitive functions. It is believed that Alzheimer’s disease initially affects neural connections involved in memory functions. Then, other regions of the brain, such as the cerebral cortex, are impacted, resulting in difficulties with language, reasoning, and social interaction.
Over time, the illness progresses to other regions of the brain, causing the incapacity to live and function without assistance. Alzheimer’s disease has a considerable mortality rate.
Chronic Inflammation and Alzheimer’s Disease
According to studies, chronic inflammation may be the source of the accumulation of glial cells that are intended to keep the brain clear of debris. The function of microglia in a healthy person is to eliminate waste and toxins. In individuals with neurological illnesses such as Alzheimer’s, however, microglia do not remove waste and debris. Additionally, it does not eliminate protein residues such as beta-amyloid plaques.
The instability of microglia is presently the focus of intensive study.
Anti-Amyloid Therapy
Experts have recently turned to amyloidogenesis in an effort to develop therapeutic pharmaceutical approaches. According to a study published in the journal Biology, such therapeutic initiatives would require the capacity to block β-sheet formation; prevent fibrillogenesis; dissolve Aβ aggregates into non-toxic species; destabilize Aβ oligomers; and accelerate the conversion of Aβ oligomers to Aβ aggregates.
More research into amyloids is warranted, however. Even though amyloids are believed to be a major contributor to the development of neurodegenerative diseases like Alzheimer’s, the reduction of Aβ-peptide production has not yielded encouraging results in clinical trials.
Alzheimer’s disease, one of the most studied illnesses of recent times, remains incurable as of the release of this publication.