Memory loss, difficulty communicating, and impaired problem-solving abilities are just some of the symptoms that can be associated with dementia, which is a general term used to describe a range of symptoms associated with a decline in cognitive ability.
It is a condition that affects the brain that is progressive and irreversible, and it can be caused by a variety of underlying conditions, such as Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, and others.
Dementia is an important condition because it diminishes a person’s capacity to carry out the activities of daily living and has the potential to have a significant negative effect on the quality of life of the affected individual. It places a significant burden on family members and caregivers, who frequently have to provide care for those who are affected around the clock.
In addition, dementia is a significant problem in terms of public health because it affects a large number of people all over the world, and that number is steadily growing, particularly as the population gets older.
According to the World Health Organization, there are currently approximately 50 million people around the world living with dementia, and it is anticipated that this number will triple by the year 2050. Because of this, dementia has significant repercussions for society, the economy, and healthcare, making the treatment of this condition a priority for the health of the entire world.
Dementia can be classified into four main types: Alzheimer’s disease, vascular dementia, Lewy body dementia, and frontotemporal dementia. Here, the four main types of dementia are described.
1. Alzheimer’s Disease
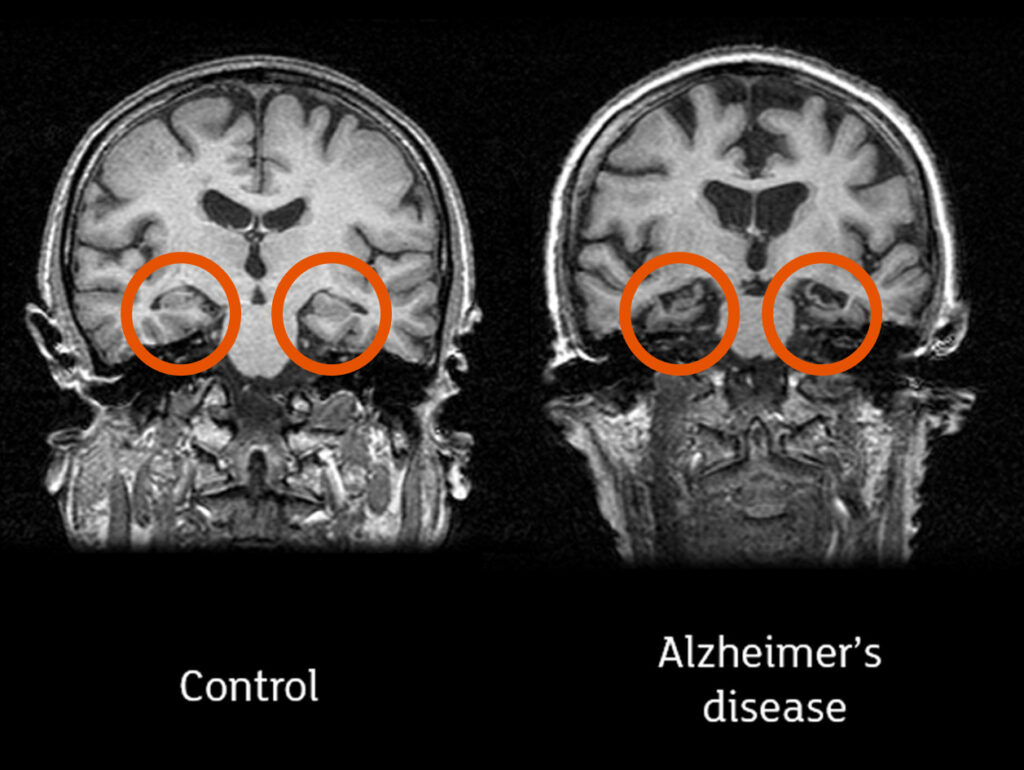
Memory, thinking, and behavior are all impacted by Alzheimer’s disease, which is a form of dementia caused by a degenerative brain disorder. It is the leading cause of dementia and is responsible for between 60 and 80 percent of all cases. Dr. Alois Alzheimer, a German psychiatrist who first described the condition in 1906, is honored with the eponymous disease that bears his name.
The History of Alzheimer’s Disease
Dr. Alois Alzheimer first became aware of the condition while observing a patient named Auguste Deter, who suffered from memory loss, trouble speaking, and delusions. After she had passed away, Dr. Alzheimer conducted an autopsy on her brain and found abnormal protein deposits, which he referred to as “plaques” and “tangles.” It is now widely accepted that Alzheimer’s disease is characterized by the presence of plaques and tangles.
Over the course of the subsequent few decades, researchers gained more knowledge about the disease and discovered that it is a progressive brain disorder that causes the death of brain cells and impairs cognitive function. The term “Alzheimer’s disease” was officially accepted by the medical community and used for the first time in 1974.
Importance of Alzheimer’s Disease Diagnosis
Because it affects such a large number of people all over the world and continues to do so, Alzheimer’s disease is a significant problem in terms of public health. According to the World Health Organization, there are currently approximately 50 million people around the world living with dementia, and it is anticipated that this number will triple by the year 2050. In the United States, Alzheimer’s disease is the sixth leading cause of death overall and the fifth leading cause of death for people aged 65 and older.
The disease has significant repercussions for society as a whole, as well as for the economy and the healthcare system. It places a significant burden on family members and caregivers, who frequently have to provide care for those who are affected around the clock. In addition, the cost of providing care for people who have Alzheimer’s disease is already quite high, and projections indicate that this cost will rise substantially as the population continues to age.
Treatments for Alzheimer’s Disease
There is currently no treatment that can reverse Alzheimer’s disease. However, there are medications that can help alleviate symptoms and improve cognitive function. These medications are currently available. These medications include cholinesterase inhibitors, which help improve memory and thinking, and memantine, which helps regulate the activity of glutamate, a neurotransmitter that is involved in learning and memory. Cholinesterase inhibitors help improve memory, and memantine helps regulate glutamate activity.
Alterations to one’s way of life, in addition to the use of medicinal treatments, may also be helpful in the management of Alzheimer’s disease symptoms. It has been shown that people who have the disease can benefit from participating in activities such as regular exercise, eating a healthy diet, and maintaining positive social relationships. In addition, there are a number of treatments that do not involve the use of drugs that can assist in improving cognitive function. Some of these treatments include cognitive rehabilitation, occupational therapy, and music therapy.
Ongoing efforts are being put into the investigation of potential new treatments for Alzheimer’s disease. There are currently a number of clinical trials being conducted to investigate potential new treatments and medications for the disease. Immunotherapy, in which abnormal protein deposits associated with Alzheimer’s disease are targeted and removed with the assistance of antibodies, is an approach that has shown some promise as a potential treatment.
In summation, Alzheimer’s disease is a progressive disorder of the brain that has an effect on a person’s memory as well as their thinking and behavior. It is the most common cause of dementia and has significant repercussions for society as a whole, the economy, and the healthcare system.
Even though there is no known cure for the disease at this time, there are treatments available, including medications, changes in lifestyle, and therapies that do not involve the use of drugs, that can help manage symptoms and improve quality of life. Ongoing research into potential new treatments provides grounds for optimism regarding the future.
2. Vascular Dementia
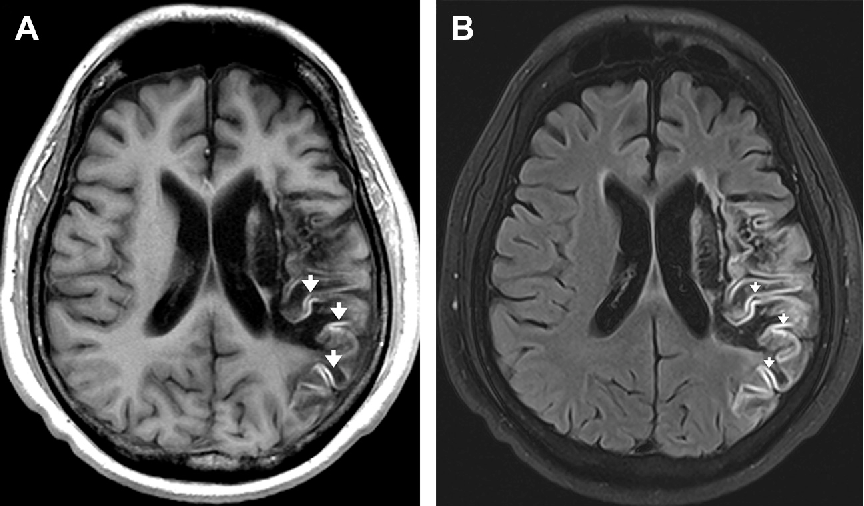
Vascular dementia is a form of dementia that manifests itself when there is damage to the blood vessels in the brain. These blood vessels are responsible for supplying the brain with the oxygen and nutrients it needs to function properly. This condition can arise following a stroke or a string of mini-strokes, and it can also result from other conditions that affect the blood vessels, such as high blood pressure or atherosclerosis.
A History of Vascular Dementia
For a long time, people have been aware that cardiovascular disease can cause dementia. In the 19th century, doctors and other medical professionals observed that patients who had suffered strokes frequently developed cognitive impairments. However, the condition wasn’t dubbed “multi-infarct dementia” until the 1960s. Prior to that, it was known as “dementia with multiple small strokes.”
Researchers eventually came to the conclusion that vascular dementia could be brought on not only by massive strokes that were easily identifiable, but also by a series of smaller strokes that occurred over the course of a person’s lifetime and went undetected. In 1997, the diagnosis of “vascular dementia” became the common practice for referring to this condition.
The Importance of Vascular Dementia
Following Alzheimer’s disease as the most common cause of dementia, the second most common cause is vascular dementia, which accounts for approximately 20% of cases. It is a significant problem for the world’s public health because it affects a large number of people all over the world, particularly as the population gets older.
The disease has significant repercussions for society as a whole, as well as for the economy and the healthcare system. It places a significant burden on family members and caregivers, who frequently have to provide care for those affected around the clock. In addition, the cost of providing care for people who have vascular dementia is already quite high, and projections indicate that this cost will rise substantially as the population continues to age.
How Vascular Dementia Is Treated
The treatment for vascular dementia is condition specific and determined by the underlying cause. It is possible to manage the condition and prevent further damage to the blood vessels by making changes to one’s lifestyle and taking medication. If the condition is caused by atherosclerosis or high blood pressure, these conditions may have caused it.
If the condition was caused by a stroke, then medication such as antiplatelet drugs or anticoagulants may be used to reduce the risk of future strokes occurring. It is possible that surgery will be required in certain circumstances in order to unblock blood vessels or repair damage to blood vessel walls.
Alterations to one’s way of life, in conjunction with conventional medical treatment, may also be helpful in the management of the symptoms of vascular dementia. It has been demonstrated that individuals who have the disease can benefit from participating in activities such as regular exercise, maintaining a healthy diet, and maintaining positive social relationships.
Rehabilitative approaches such as cognitive therapy, occupational therapy, and speech therapy may also be helpful in the management of symptoms associated with vascular dementia. These therapies may assist in the improvement of cognitive function, communication skills, and other skills necessary for day-to-day living.
In conclusion, vascular dementia is a form of dementia that takes place when there is damage to the blood vessels that supply the brain with oxygen and nutrients. This damage can take place as a result of a number of different conditions. It is the second-most common cause of dementia, behind Alzheimer’s disease, and it has significant repercussions for society, the economy, and the healthcare system.
The treatment for vascular dementia is determined by the underlying cause of the condition and may involve medication, surgery, adjustments to the patient’s way of life, and therapies designed to improve cognitive function and skills necessary for day-to-day living. Early diagnosis and treatment are critical for enhancing both the prognosis and the quality of life for patients suffering from any form of dementia.
3. Frontotemporal Dementia
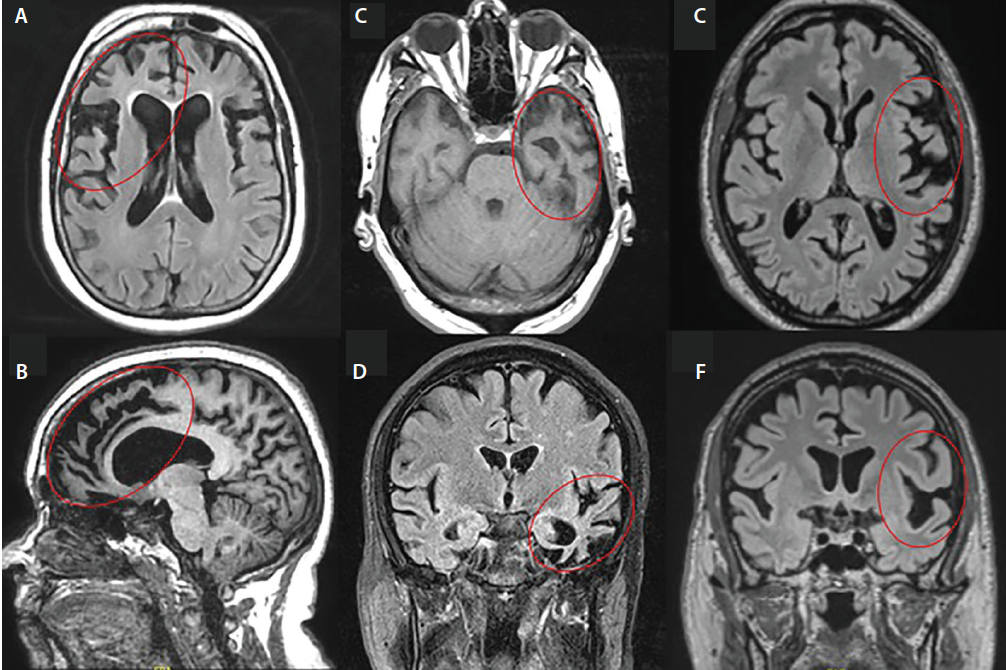
The terms frontotemporal dementia (FTD) and frontotemporal lobar degeneration (FTLD) are used interchangeably to refer to the same group of disorders that are characterized by the progressive degeneration of the frontal and temporal lobes of the brain. Pick’s disease is a common name for the condition, which is also known as frontotemporal lobar degeneration (FTLD). Arnold Pick, who was the first person to describe the disorder in 1892, is named after the disease.
A History of Dementia With Frontotemporal Degeneration
When researchers in the 1960s observed a distinct pattern of behavior and language impairment in patients with dementia, they came up with the concept of frontotemporal dementia (FTD) for the first time. Researchers were able to pinpoint the specific brain areas affected by FTD in the 1980s thanks to advancements in brain imaging, which improved understanding of the condition. This led to a better understanding of the disease.
Researchers have, over the course of their work, uncovered several distinct subtypes of FTD. These subtypes include primary progressive aphasia (PPA), behavioral variant frontotemporal dementia (bvFTD), and semantic dementia. Each subtype differs from the others in terms of its unique set of symptoms and brain alterations.
Importance of Frontotemporal Dementia
It is estimated that FTD is responsible for anywhere from 10 to 20 percent of all instances of dementia. This type of dementia, which is also the most prevalent type in people under the age of 60, most frequently affects people under the age of 65.
The fact that FTD can be difficult to diagnose due to the fact that it can be mistaken for other neurological and psychiatric conditions makes it an important condition. The condition can have a significant impact on a person’s behavior, language, and social interactions, which can lead to significant changes in both the person’s personality and their relationships with other people.
Alzheimer’s Disease and Frontotemporal Dementia Treatment
Since there is currently no treatment that can reverse the effects of FTD, the primary goal of medical intervention is to alleviate its symptoms. Behavioral symptoms such as aggression, anxiety, and depression can be managed with the help of medications such as antidepressants, antipsychotics, and mood stabilizers. In addition, behavioral symptoms can be managed through behavioral therapy.
People who have PPA may benefit from speech and language therapy as well, as this type of treatment can assist them in maintaining their communication abilities and overall quality of life. It is possible for people living with FTD to benefit from occupational therapy and physical therapy, both of which can help them maintain their independence and improve their quality of life.
Surgery is an option for treating the symptoms of frontotemporal dementia in some patients. Deep brain stimulation (DBS), for instance, is a surgical procedure that involves implanting electrodes in specific regions of the brain to improve motor function and reduce symptoms such as tremors and stiffness. DBS is one example of a treatment for Parkinson’s disease.
In summary, frontotemporal dementia is a group of disorders that is characterized by the progressive degeneration of the frontal and temporal lobes of the brain. This degeneration can occur at any age. It is a significant cause of dementia, particularly in younger people, and it can have a significant impact on a person’s behavior, language, and social interactions. The risk of developing dementia increases with age.
Although there is currently no treatment that can reverse the effects of FTD, its symptoms can be managed through a combination of medication, therapy, and even surgery. In order to improve outcomes and quality of life for people who have FTD and their families, early detection and management of symptoms are essential components.
4. Lewy Body Dementia
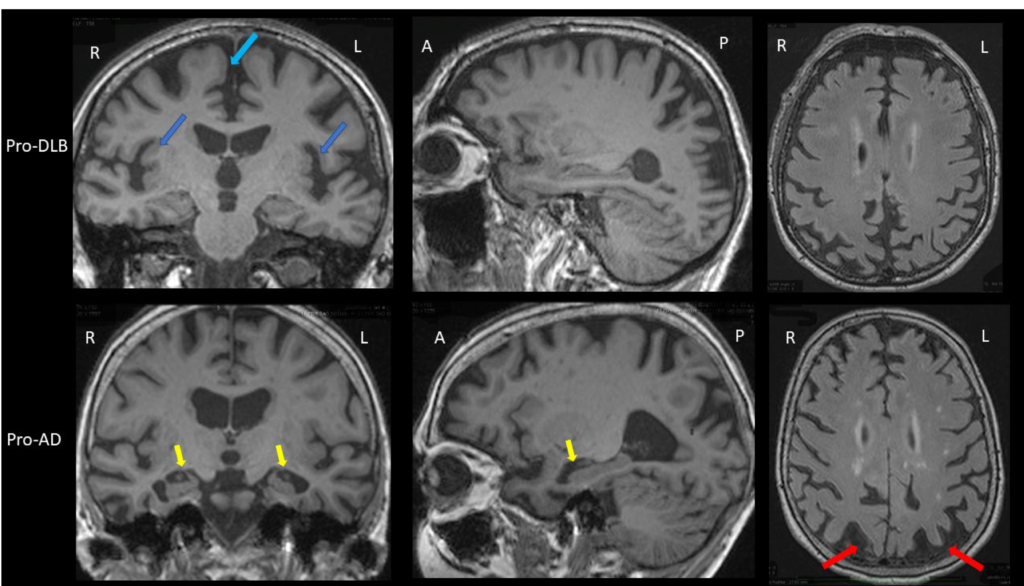
Lewy body dementia (LBD) is a progressive dementia that is characterized by the abnormal accumulation of Lewy bodies, also known as alpha-synuclein protein deposits, in the brain. The condition is also referred to as dementia with Lewy bodies or Lewy body disease from time to time.
The History of Lewy Body Dementia
Frederic Lewy, a German neurologist, was the first person to ever propose the idea of LBD. He did this sometime in the early 1900s. He was also the one who discovered the abnormal protein deposits that now bear his name. In spite of this, it wasn’t until the 1960s that researchers started recognizing LBD as its own distinct form of dementia.
The two primary subtypes of LBD that researchers have identified over time are dementia with Lewy bodies (DLB) and Parkinson’s disease dementia (PDD).Both subtypes exhibit many of the same symptoms and brain changes, but the onset of those symptoms and changes occurs at different times in both cases.
importance of Lewy Body Dementia
LBD is a significant factor in the development of dementia and is responsible for up to 10–15% of all instances of the condition. People over the age of sixty are most likely to be afflicted with it, and men are more likely than women to suffer from it.
LBD is significant because it can be difficult to diagnose because it can mimic other neurological and psychiatric disorders. This is one of the reasons why it is so important. The condition can have a significant impact on a person’s cognitive function, motor function, and behavior, which can lead to significant changes in both the person’s personality and the relationships they have with other people.
The Treatment of Lewy Body Dementia
Since there is currently no treatment that can reverse the effects of LBD, the primary goal of medical intervention is to alleviate its symptoms. To improve cognitive function and manage behavioral symptoms like agitation, hallucinations, and delusions, it is possible to use medications like cholinesterase inhibitors and memantine. These types of drugs inhibit the enzyme cholinesterase.
The management of the motor symptoms of LBD, such as tremors and stiffness, may also benefit from the utilization of physical therapy and exercise. The management of communication difficulties, as well as the preservation of one’s quality of life, may benefit from speech and language therapy.
Deep brain stimulation (DBS) is a potential treatment option for managing the motor symptoms of LBD in some patients. The deep brain stimulation (DBS) procedure entails implanting electrodes in particular regions of the brain in order to improve motor function and reduce symptoms like tremors and stiffness.
It is essential to be aware that some pharmaceuticals, such as antipsychotics, have the potential to aggravate the symptoms of LBD and should be avoided whenever it is practicable to do so. In order to effectively manage the symptoms of LBD and improve outcomes for patients as well as their families, support and education for caregivers are also essential components.
To sum up, Lewy body dementia is a type of progressive dementia that stands out due to the accumulation of abnormal protein deposits in the brain. It is a significant factor in the development of dementia, especially in older adults, and it has the potential to have a significant influence on the cognitive function, motor function, and behavior of a person.
Although there are no interventions that can reverse the effects of LBD, the symptoms can be managed through a combination of medication, therapy, and even surgery. In order to improve outcomes and quality of life for people living with LBD and their families, early detection and management of symptoms are essential components.